
Background
Methods
Findings
Interpretation
Funding
Introduction
Previous studies, including analyses from the COVID-19 Global Rheumatology Alliance physician registry, have reported associations between worse COVID-19 outcomes in patients with rheumatic disease and the following risk factors: older age, a high burden of comorbidities, high doses of glucocorticoids, high disease activity, and the use of particular conventional synthetic disease-modifying anti-rheumatic drugs (DMARDs) and biological and targeted synthetic DMARDs.
,
,
However, patients with rheumatic diseases differ greatly in their demographic profiles and in their exposure to immunosuppressive therapies.
It is therefore important to understand the factors associated with poor COVID-19 outcomes in patients with primary systemic vasculitis. Similar to these patients, those with polymyalgia rheumatica might also be at high risk for poor COVID-19 outcomes, given that they have similar age demographics and also receive long-term treatment with glucocorticoids.
The outcomes of COVID-19 in this patient population have not yet been reported.
Methods
Study design and participants
,
,
,
,
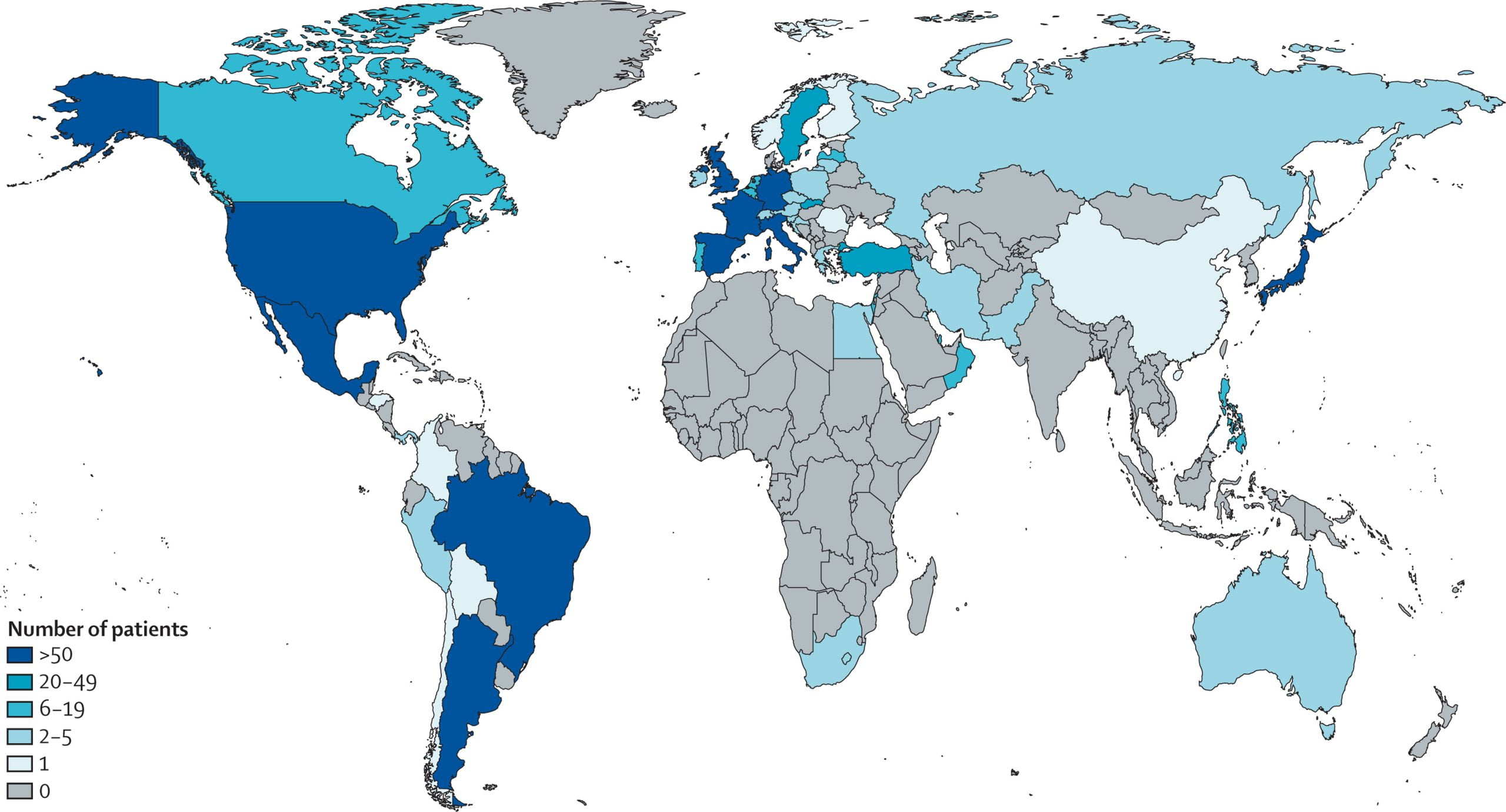
Cases are voluntarily entered by rheumatologists or other health-care providers. Data are entered directly into the global or European data entry systems, or transferred from national registries (France, Germany, Italy, Portugal, or Sweden). Patients aged 18 years and older diagnosed with COVID-19 (confirmed or presumptive) between March 12, 2020, and April 12, 2021, who had a history of primary systemic vasculitis or polymyalgia rheumatica were included. Primary systemic vasculitis included antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (granulomatosis with polyangiitis, microscopic polyangiitis, or eosinophilic granulomatosis with polyangiitis), giant cell arteritis, Behçet’s syndrome, and other vasculitides including Kawasaki disease. A text entry option was available when inputting data to the registry to provide a specific diagnosis or another diagnosis, if not listed. Data quality was assessed by the University of California (San Francisco, CA, USA) and the University of Manchester (Manchester, UK), both of which confirmed that there were no duplicates in the data entries. Given the nature of the data collected, the UK Health Research Authority and the University of California San Francisco institutional review board considered this study exempt from the need to obtain patient consent. Both institutions provided ethics approval for this study.
Procedures
comorbidities (hypertension, cardiovascular disease, diabetes, chronic kidney disease, lung disease, interstitial lung disease, or cancer), number of comorbidities (analysed as a continuous variable), body-mass index (BMI; obese [BMI ≥30 kg/m2] or non-obese [BMI <30 kg/mg2]), smoking status (ever or never smoker), disease activity, as per the physician’s global assessment (remission, low, moderate, or high or severe), and region (Europe, North America, South America, or other). Other regions included Asia, Eastern Mediterranean, South-East Asia, and Western Pacific region.
Statistical analysis
,
We also did a sensitivity analysis including independent comorbidities (hypertension, cardiovascular disease, diabetes, chronic kidney diseases, lung disease, or interstitial lung disease) in patients with ANCA-associated vasculitis. Results were considered statistically significant at a two-sided p value of less than 0·05. Analyses were done in R, version 4.0.2.
